Patterns of health and disease are determined by the social, political, and economic systems that govern the world we live in. The current coronavirus disease (COVID-19*1) pandemic is no exception to this. Our growing global connectedness through increasing transnational and transcontinental traffic and trade has made us vulnerable to the spread of novel pathogens (new disease-causing agents). The sheer volume of literature and films outlining hauntingly similar fictitious parallels – or apparent predictions – of the ongoing COVID-19 pandemic is testament to the extent to which we were already aware of both the threat of novel pathogens and the potential vulnerabilities of our own systems for global preparedness and response.
International Health Regulations and global governance
Coming in the wake of the 2002–2004 SARS coronavirus (SARS-CoV-1) epidemic that affected 29 countries and territories, but predominantly China, Hong Kong, Taiwan, Canada and Singapore,*2 the 2005 International Health Regulations (IHR [2005]) set out with the explicit purpose to “help the international community prevent and respond to acute public health risks that have the potential to cross borders and threaten people worldwide.”*3 Prior international regulations, dating back to the first International Sanitary Conference in Paris in 1851, had focused on lists of priority infectious diseases requiring standardized international procedures for their effective control and the prevention of cross-border spread. By the 1952 International Sanitary Regulations, specific procedures for quarantine and international notification to the World Health Organization (WHO) had been outlined for plague, cholera, yellow fever, smallpox, typhus and relapsing fever, in addition to more general sanitary requirements related to international transport and points of entry.*4 By comparison, IHR (2005) broadened the scope of public health events beyond known infectious agents in a bid to address emerging infectious diseases as well as events with major implications for the health of populations that are unrelated to biological pathogens (viruses, bacteria, etc.), such as the release of radioactive materials or toxic chemicals into the environment. The spread of HIV/AIDS from the 1980s and civil society attention on the threats of nuclear technology and chemicals pointed to the need for stronger international regulations that would address the full spectrum of public health risks in modern society.
The first International Sanitary Regulations in the mid-nineteenth century aimed to standardize isolation and quarantine procedures to reduce the spread of communicable diseases across borders and the propagation of epidemics. These regulations foreshadowed the establishment of the World Health Organization, which today plays a central role in global governance to effectively prevent, detect, and respond to potential pandemics.
IHR (2005) places obligations on states to report to WHO any event that might constitute or risk becoming a global health emergency. A number of criteria are involved in such an assessment by states, including whether the event is sufficiently serious, unexpected, significant enough to spread internationally, or significant enough to affect international trade. Under IHR (2005), WHO may consider unofficial reports of such events and seek verification from states. Moreover, once such information is received, the Director-General of WHO, Dr. Tedros Adhanom Ghebreyesus, must decide whether the apparent risks to public health warrant the convening of an Emergency Committee, which will advise whether the situation constitutes a global health emergency (a public health emergency of international concern, in the language of the IHR [2005]). Once this is declared, the Emergency Committee, comprising international experts, provides advice on temporary recommendations needed to control the situation and eventually is responsible for determining when the global health emergency is over. The Emergency Committee for Pneumonia due to the Novel Coronavirus 2019-nCoV was convened on January 22, 2020 and advised to declare the situation a global health emergency on January 30. WHO Director General’s announcement on March 11 that COVID-19 constitutes a pandemic underscored the seriousness of the current situation but did not have additional implications for the international mechanisms already activated.
WHO response to global health emergencies
WHO’s Emergency Response Framework determines the organization’s functions and guides its actions during any emergency situation. As the United Nations specialized agency for health, WHO works to support state emergency responses to public health events, in line with its core emergency functions: leadership; partner coordination; information and planning; health operations and technical expertise; operations support and logistics; and finance and administration. In a public health emergency of international concern, additional functions of the organization are activated. In terms of leadership and coordination, WHO’s Director General activates the Emergency Committee, which strengthens the coordinated assessment of evidence and dissemination of expert technical guidance to support the country-level and international response. WHO operates the Global Outbreak Alert and Response Network, which promotes sharing of information from states to facilitate planning, preparedness, and interventions. In times of a global health emergency, specific information-sharing platforms are created, as with WHO’s designated coronavirus platform and interactive map to monitor case incidence and deaths globally. The critical functions of operations, logistics, administration, and finance work overboard. Usually unseen by the general public, these teams are the unsung heroes of global health emergencies who have to find solutions to considerable barriers such as market shortages of personal protective equipment so desperately needed in the frontline response.
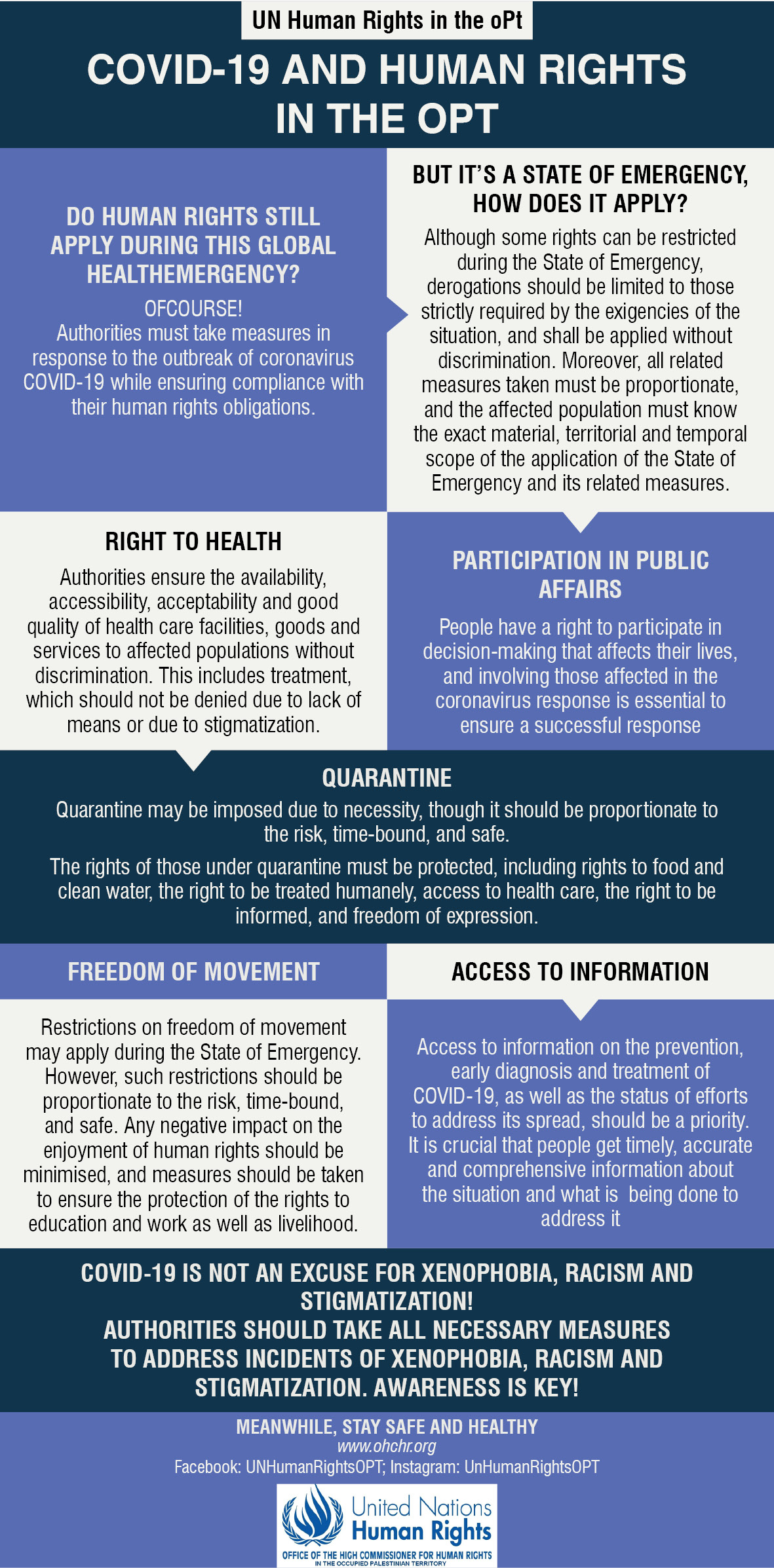
Protection and respect for human rights are integral to WHO’s Emergency Response Framework and IHR (2005). As outlined by UN Human Rights Palestine, human rights still apply during emergency situations. Any restriction of rights, such as limitations on free movement, should be implemented without discrimination, be proportionate to the risk, and safe. Negative impacts on the enjoyment of rights, including the right to access health services and to wider determinants of health such as rights to work and to earn a living, should be minimized.*5
What international recommendations are currently in place for COVID-19?
Coronavirus disease is an infection that mainly affects the respiratory tract. This means from your nose and mouth to your lungs. The infection is spread through inhaling droplets breathed or coughed out by someone with COVID-19 or touching contaminated surfaces and then touching your eyes, nose, or mouth. The mechanisms of spread are significant because they give us an indication of what kinds of intervention are effective for preventing the disease. While governments have differed in the level of their responses to isolate and contain the virus, the principles informing responses are the same. For individuals, WHO advises that you can reduce your chances of catching or spreading COVID-19 by frequently washing your hands, maintaining social distancing (both keeping a distance during social interactions and reducing the frequency of those interactions), avoiding touching your eyes, nose, and mouth, practicing respiratory hygiene (covering your nose and mouth with your bent elbow when you cough or sneeze), and seeking medical attention and self-isolating when you have symptoms of a cold, cough, or fever.*6 State regulations to quarantine those at higher risk of having been exposed, isolate people with symptoms, and reduce social gatherings, interactions, and travel are additional measures to try to reduce the spread – or rate of spread – of the disease, and to prevent the overwhelming of limited healthcare resources.
You can reduce your chances of catching or spreading COVID-19 by frequently washing your hands, maintaining social distancing, avoiding touching your eyes, nose, and mouth, practicing respiratory hygiene, and seeking medical attention and self-isolating when you have symptoms of a cold, cough, or fever.
COVID-19 has proved harder to contain than previous coronaviruses outbreaks, including SARS-CoV-1 and MERS-CoV. COVID-19 is spread from one person to another even if that person has only mild symptoms. There have also been reports of spread of the virus before people show symptoms, but this is not the main way the virus is spread – and people are most contagious when symptomatic.*7 It is also more contagious at the time when a person has first been infected. By contrast, we know that the peak shedding of virus (and infectivity) for SARS-CoV-1 occurred later in the course of illness, and when people had more severe infections of the lungs.*8 Studies that focused on the characteristics of the COVID-19 outbreak in China have estimated the basic reproduction number (R0) to be between around 2.0 and 3.5.*9 This means that for every person infected in a completely susceptible population, you would expect between 2 and 3.5 other people to become infected. To cause an outbreak (epidemic), this number must be more than 1. The most infectious virus to affect humans, measles, has a basic reproduction number of approximately 15 (11 to 18).*10 When the reproduction number is less than 1, the infectious agent cannot cause an outbreak; less than one additional person will catch the disease for every initial person affected, so the disease dies out.
The basic reproduction number of COVID-19 has been the basis of some worst-case projections – since it indicates exponential growth – but there is a critical difference between the basic (theoretical) reproduction number and the effective one, that is the number of the real population (susceptible and immune) that become infected over time. The effective reproduction number depends on a population’s susceptibility (where previous exposure and vaccination leads to immunity) and its dynamic characteristics. With the example of measles, the effective reproduction number is brought to less than 1 through mass vaccination.
With the current COVID-19 pandemic, our behaviors to maintain hygiene and distance ourselves from one another also bring the effective reproduction number down. The aim is to reduce the reproduction number of the virus in order to slow spread to the extent that we don’t go over a threshold that would overwhelm demand on health services (“flatten the curve”) and that would eventually lead to elimination of the virus (when reproduction number becomes less than 1). Because COVID-19 disease has not been observed before, we are still learning which interventions are most effective. Broadly, early detection; availability of adequate medical supplies; admission to hospital for treatment of severe cases;*11 personal and collective hygiene;*12 and reducing the frequency of social interactions through isolation, quarantine, social distancing and community containment*13 are so far understood to be effective.
How can we prevent, detect and adequately respond to similar events in the future?
IHR (2005) include state obligations to develop core public health capacities that are the minimum necessary for adequate prevention, detection, and response to any potential global health emergency. WHO provides technical guidance and support to states to assess current capacities and inform strengthening efforts related to national legislation, coordination, surveillance, laboratories, reporting, human resources, emergency preparedness, and response. On the basis of lessons learned from the 2014–2016 Ebola global health emergency, WHO developed the Joint External Evaluation tool*14 to assist the impartial assessment of current country-level public health systems and inform efforts to build capacity. In Palestine, a joint external assessment was carried out in 2016, which served as the basis of the IHR action plan from 2017. The next joint evaluation is due for 2020. As with all development efforts, the success of such initiatives depends on more than technical assessment. It needs political commitment and the availability and continued production of adequate resources – in terms of financing, supplies, equipment, and staff.
The occupied Palestinian territory faces unique challenges to sustainable financing and provision of its public health system, with lack of Palestinian sovereignty or control over movement and natural resources, and high donor dependency. Movement restrictions and fragmentation of territory and healthcare provision hamper the effective response to public health emergencies. The susceptibility of the Gaza Strip to a devastating outbreak is particularly concerning, with overcrowding, limited access to clean water and adequate sanitation for large sections of the population, and an already overstretched health system in the wake of more than 12 years of blockade, successive conflicts, and the large numbers of severe injuries sustained during the Great March of Return.
The current COVID-19 pandemic lays bare our shared humanity and shared vulnerability. The increased susceptibility of populations with fewer resources and reduced capacity for preparedness, detection, and response underlines the extent to which our health is determined by social, political, and economic forces. Strengthening our current response to and future prevention of global health emergencies is a collective responsibility. Realizing that responsibility, in Palestine and elsewhere, requires internationalism, mobilization, and solidarity in times of crisis and times of calm to protect health and human rights and to bring about justice and dignity for all.
*1 The virus itself is called SARS-CoV-2, but to avoid confusion, I use COVID-19 to refer to the disease and virus in this article.
*2 WHO, 2003, “Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003.” Available at https://www.who.int/csr/sars/country/table2004_04_21/en/ (accessed 13.3.20).
*3 WHO, 2016, International Health Regulations (2005) Third Edition.
*4 WHO, 1952, “International Sanitary Regulations.” Available at https://apps.who.int/iris/bitstream/handle/10665/85636/Official_record37_eng.pdf?sequence=1&isAllowed=y (accessed 13.3.20).
*5 OHCHR Palestine, 2020, “COVID-19 and human rights in the oPt.” Available at https://www.facebook.com/UNHumanRightsOPT/photos/a.580351668819829/1365669283621393/?type=3&theater (accessed 13.3.20).
*6 WHO, 2020, “Coronavirus disease (COVID-19) advice for the public.’ Available at https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed 13.3.20).
*7 CDC, 2020, “Coronavirus disease 2019 (COVID-19), How to Prepare: How It Spreads.” Available at https://www.cdc.gov/coronavirus/2019-ncov/prepare/transmission.html (accessed 20.3.20).
*8 H. Branswell (2020), “People ‘shed’ high levels of coronavirus, study finds, but most are likely not infectious after recovery begins.” STAT News Health. Available at https://www.statnews.com/2020/03/09/people-shed-high-levels-of-coronavirus-study-finds-but-most-are-likely-not-infectious-after-recovery-begins/ (accessed 13.3.20).
*9 Y. Wang, et al (2020), “Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures.” Journal of Medical Virology.
*10 F.M. Guerra et al (2017), “The basic reproduction number (R0) of measles: a systematic review.” Lancet Infectious Diseases.
*11 Fang et al, 2020, “Transmission dynamics of the COVID-19 outbreak and effectiveness of government interventions: A data-driven analysis.” Journal of Medical Virology.
*12 WHO, 2020, “Coronavirus disease (COVID-19) advice for the public.” Available at https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed 13.3.20).
*13 A. Wilder-Smith and D.O. Freedman (2020), “Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak.’ Journal of Travel Medicine.
*14 WHO, 2018, “Joint external evaluation tool: International Health Regulations (2005),” second edition. Available at https://apps.who.int/iris/bitstream/handle/10665/259961/9789241550222-eng.pdf?sequence=1 (accessed 13.3.20).